A standard IVF cycle begins with the female partner starting ovarian stimulation, carefully managed by a fertility specialist. The goal of ovarian stimulation is to produce more eggs (oocytes) than are normally produced during a natural cycle. At the end of the stimulation, all the oocytes are collected through a procedure called ‘oocyte pick up’ (or OPU). At the same time, the male partner is assessed to determine the best way to obtain a viable sperm sample, which will either by masturbation, aspiration of the testes, or through surgical collection. However, the most common way is through masturbation. With the collection of the female and males gametes complete, the focus of the cycle shifts to the embryology laboratory.
The embryology laboratory at Westmead Fertility Centre contains the most advanced assisted reproductive technology (or ART) equipment available and it is where the latest, research driven, scientific procedures are used to assist our patients in realising their dreams of becoming parents.
Preparing the gametes (the oocyte and sperm)
On the day of the OPU procedure (in the Ambulatory Surgical Unit of Westmead Hospital), one of our gynaecologists (supported by an anaesthetist to make sure you are comfortable) will aspirate the follicular fluid from the stimulated ovarian follicles. The follicular fluid is immediately examined by one of our highly trained embryologists who will identify whether any oocytes are contained in the fluid. It is important to remember that not all follicles will contain an oocyte. The embryologist identifies the oocyte(s) in the fluid by using a sterile microscope equipped with a heated stage. Oocytes are very sensitive to changes in temperature and one of the main jobs of the embryologist is to ensure that the oocytes are handled as close to body temperature (37°C) as possible. As the oocytes are located, they are transferred into a specialised kind of solution (medium) and stored in a controlled environment until the end of the procedure.
A specialised portable incubator is used to keep the oocytes safe, secure, and in an environmentally controlled sterile condition while they are brought to our embryology laboratory. Cumulus cells surround the freshly collected oocytes and together they are known as cumulus-oocyte complexes (or COC). The COC are washed and cleaned in the laboratory and placed in fresh culture medium in an incubator waiting for the fertilisation step.
Whilst the OPU is being performed, the sperm sample is collected and then examined in our andrology laboratory to determine the best way to prepare the sample. The most advanced techniques are used to extract the most active, mature, and morphologically normal sperm to be used to fertilise the oocytes.
Fertilisation of the egg (oocyte) by the sperm
Depending on the quality and activity of the sperm within the sample, our highly trained embryologists decide the optimum method to be used in order to fertilise the oocytes. Fertilisation can be accomplished by two different assisted reproductive technologies:
- In Vitro Fertilisation (IVF), or
- Intracytoplasmic Sperm Injection (ICSI).
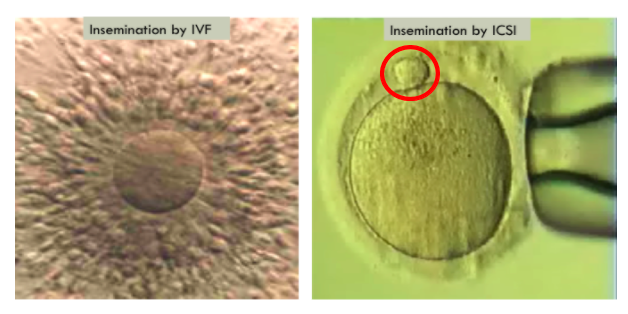
For IVF, the healthiest motile sperm are isolated and gently placed in a laboratory dish with the COCs. The sperm will surround the COCs and a single leading sperm will enter the oocyte. This triggers a chemical reaction in the zona pellucida (the shell) of the oocyte that prevents any other sperm from progressing and ensures that each oocyte is only fertilised by one sperm.
ICSI is commonly used when we don’t have enough sperm, if the sperm have low motility, or if the sperm have abnormal morphology. Instead of the sperm naturally penetrating the oocyte, a single healthy sperm is selected by one of our embryologists and injected into the cytoplasm of each mature oocyte. In order to do that, we need to remove the cumulus cells surrounding the oocytes to allow us to first determine their maturity, because only mature oocytes can be injected on the day of the oocyte collection. The maturity of the oocytes is determined by looking for the polar body (circled red in the below picture) outside the oocyte cytoplasm. The injection process is carried out using an advanced, heated, inverted microscope. The microscope is equipped with micromanipulators so the embryologist can handle and control the injection process and avoid any kind of stress to the gametes (eggs and sperm) during the procedure.
At Westmead Fertility Centre, our embryologists will assess the quality of the sperm obtained on the day to determine the technique required for optimal fertilisation. This is quite different to many other clinics where the embryologists take a more standard / less personalised approach to fertilisation and use ICSI for almost everyone.
Culturing the embryos
After IVF or ICSI, we incubate the dishes containing oocytes and sperm – supported by a solution (culture medium) – and allow fertilisation to continue for the next 18 hours.
A note on culture medium: Culture medium is a specially created solution that contains all the nutrients that the oocyte(s) and embryo(s) need while developing. The dishes containing the embryos and culture medium are carefully maintained in an incubator with very precise control over the atmosphere (gas concentrations), humidity and temperature to mimic the environment in the fallopian tubes and in the uterus. At Westmead Fertility Centre, we use the most advanced culture medium to give our patients the best chance of success.
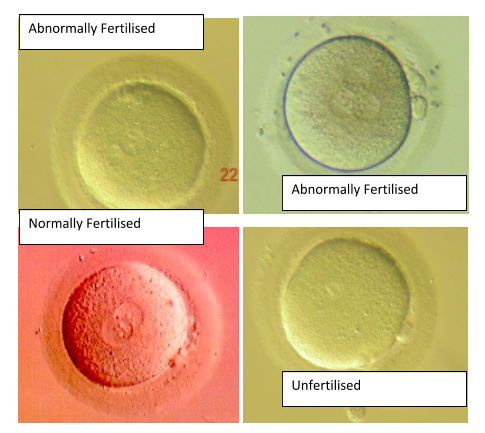
Once fertilisation has taken place, the fertilised eggs are transferred to a new specialised culture medium to support the next stage of their development and growth into a blastocyst. At the fertilisation check, the embryologists see a variety of stages of oocyte development and different types of fertilisation. Immature oocytes are occasionally seen and these types of oocytes do not have any potential to become fertilised. Also, abnormal fertilisation can be seen, where there are either too many or too few nuclei. Abnormally fertilised oocytes cannot usually be used for treatment. In general, it is expected that around 50% of the total oocytes will be fertilised normally.
Embryo development
Embryos are extremely sensitive to changes in their environment. Even the smallest disruptions can decrease the viability of the embryo and affect the chances of it becoming a baby. Our embryology team closely examine and record the embryo’s development while it is growing in our laboratory. This requires a careful balance between the need and benefit of assessment, while making sure we don’t cause unnecessary stress by taking the embryos outside of the incubator. The days and stages in which we examine the embryos will be based on each patient’s individual treatment plan.
The day after fertilisation, often referred to as day two, our embryologists are looking for the embryos to have 4 cells, growing to an 8-cell embryo on the third day, and a 16-cell embryo on the fourth day, before they start to compact in a structure called a morula, and become a blastocyst with roughly 200 cells on the fifth day. Our embryologists are highly trained to be able to track embryo development and determine which embryo will give the best chance of achieving a viable pregnancy.
Fertilisation check
Day 2: 4 cells
Our embryologists also monitor the embryos to see how healthy they are looking. At the early cleavage stage (day 2 and day 3), the cells should be smooth, round, and symmetrical, with no or few fragments broken off. Embryos with extensive fragmentation have a lower potential for producing pregnancy. At the blastocyst stage (day 5) our embryologists check that all the necessary structures are in place, such as an inner cell mass (ICM), which will grow into the foetus (baby), and an outer layer of cells called the trophectoderm (TE), which will grow into the placenta. Using these observations, our embryologists will assign a morphological grade to each embryo. For patients having blastocyst transfer we do not disturb the embryos on day two and day four, but rather leave them to grow stress-free in order to maximise their chances.
Day 3: 6 – 8 cells
Day 4: Morula
Day 5: Blastocyst
Embryo grading
Every embryology laboratory has its own method of grading embryos, and its importance lies in our ability to consistently communicate and record the development of the embryos.
At Westmead Fertility Centre we use a well-developed scoring system to describe the quality of the embryos. For example:
- 4AA – this is a fully expanded blastocyst with an excellent appearing ICM and TE
- 4AB – this is a fully expanded blastocyst with an excellent appearing ICM and good TE
- 3CC – this is an unexpanded blastocyst with a poor appearing ICM and TE
Our embryology lab evaluates each blastocyst depending on the extent of expansion with numbers 3, 4, 5, compaction and number of the cells forming the ICM with letters A, B, C, and the TE number of cells with letters A, B, C as well. This scoring system evaluates the morphological quality of the embryos. For example, a top-quality embryo will be graded 5AA, though few embryos receive this high grade. Embryos 3BC and higher have an excellent chance of resulting in pregnancy. Top-quality blastocysts have a 45-65 percent chance of resulting in pregnancy, depending on the age of the woman.
It is really important to focus on your own embryos and not compare the grading of yours to those of others. Not every top-quality embryo has the potential to create a viable pregnancy, and some poor-quality embryo’s do. The quality of the resultant embryos are a combination of many factors, the most important of which are the oocyte and sperm quality, in addition to the laboratory culture system.
Preimplantation Genetic testing PGT
Preimplantation Genetic Testing (PGT) is designed for patients requiring genetic testing of their embryos. This can be for a variety of reasons and should be something you have discussed with your Fertility Specialist prior to starting your IVF cycle. During the PGT process, one of our embryologists will biopsy (remove) a small number of cells from the embryo, and send the biopsied cells to the Genetic testing laboratory. The Genetic laboratory will check if the DNA from those biopsied cells have the right number of chromosomes (for PGT-A) or carry a known genetic condition or disease (for PGT-M), or even a combination of both.
If embryos are biopsied, they can be safely stored separately in a frozen state while the genetic testing is being done.
Noting, at this time, Westmead Fertility Centre does not offer PGT.
Embryo selection and transfer
If PGT testing is used, then the selection of embryos is already determined and the healthy and unaffected embryos are identified for embryo transfer.
Otherwise, our embryologists will use their experience and our scoring system to assess the appearance of the embryo, and review its developmental history, in order to select the best embryo for transfer. At Westmead Fertility Centre we will transfer embryos on day 2, 3, and 5 to give our patients the best chance of achieving a pregnancy. Choosing the optimum day for the embryo transfer depends on many factors, like the number of fertilised oocytes seen on day one, how these embryos are growing, and their quality.
Some members of our scientific team at Westmead Fertility Centre
Choosing a clinic to help you
At Westmead Fertility Centre, your baby is our only goal and science is how we achieve it. As you can see, growing each individual embryo takes an exact science to get it right. And, each precious embryo needs a good embryology laboratory, with excellent culture conditions, and well-trained and experienced embryologists to ensure your success. All of our embryologists are educated to at least Masters level, with a senior team that can draw on vast experience at both a national and international level.
Learn more about our Scientific Director, A.Professor Cecilia Sjoblom here: https://www.westmeadfertilitycentre.com.au/meet-westmead-fertility-centres-scientific-director-associate-professor-cecilia-sjoblom/
All content should be considered as opinion only. Always seek the direct advice of your doctor in connection with any questions or issues you may have.
















